Anthrax
Anthrax is an infection caused by the bacterium Bacillus anthracis. It typically affects the skin, lungs, or intestines, and can occur through contact with infected animals or animal products. Symptom onset varies from one day to over two months post-exposure.
Signs and Symptoms
Skin

Cutaneous anthrax, also known as hide-porter's disease, is the most common form, accounting for over 90% of cases. It presents as a boil-like skin lesion that eventually forms a painless ulcer with a black centre (eschar). Nearby lymph nodes may become infected, swollen, and painful.

Injection

Injected anthrax may resemble cutaneous anthrax but lacks black eschar and can cause deep muscle infections, spreading faster and making it harder to recognise and treat.
Lungs
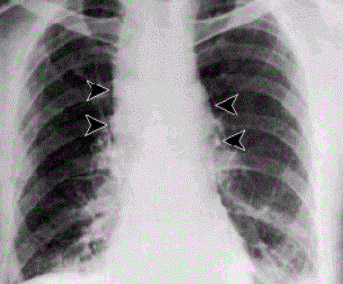
Inhalation anthrax develops within a week to two months. Early symptoms are non-specific, resembling influenza, including fever, chills, fatigue, cough, and chest pain. Later stages include severe respiratory distress, high fever, and shock.
Gastrointestinal
Gastrointestinal anthrax is caused by consuming contaminated meat and presents with severe diarrhoea, abdominal pain, and vomiting. Lesions may be found in the intestines, mouth, and throat.
Cause
Bacteria

Bacillus anthracis is a rod-shaped, Gramme-positive, facultative anaerobe. It forms hardy spores that can survive in the soil for decades. Infection occurs when spores enter the body through inhalation, ingestion, or open wounds.
Diagnosis
Diagnosis involves identifying B. anthracis in clinical material via Gramme staining, polymerase chain reaction assays, or immunofluorescence microscopy. Rapid diagnostic techniques and culturing on specific media like sheep blood agar are standard practices.

Prevention
Vaccines
Vaccination is recommended for high-risk individuals, with the current FDA-approved vaccine being BioThrax. This vaccine is administered in a series of five doses with annual boosters.
Antibiotics
Preventive antibiotics such as ciprofloxacin or doxycycline are recommended for those exposed to anthrax. Early detection and prophylactic antibiotic treatment are very important.
Treatment
Antibiotics
Early treatment is essential, involving intravenous and oral antibiotics like ciprofloxacin, doxycycline, erythromycin, vancomycin, or penicillin.
Monoclonal Antibodies
Raxibacumab and obiltoxaximab are FDA-approved monoclonal antibodies that neutralise B. anthracis toxins, used in conjunction with antibiotics to treat inhalational anthrax.
Prognosis
Cutaneous anthrax has a low fatality rate if treated, but inhalational anthrax has a higher mortality rate, even with treatment. Gastrointestinal anthrax has a fatality rate of 25% to 60%, depending on treatment timeliness.
Epidemiology
Globally, at least 2,000 cases occur annually. In the United States, cases are rare, with isolated incidents linked to occupational exposure or contaminated animal products.
History
Discovery
Robert Koch first identified B. anthracis in 1875, and Louis Pasteur developed the first effective vaccine in 1881. Since then, various strains have been studied and used, including in bioweapons programmes.

Biological Warfare
Anthrax spores have been used as bioweapons, with notable incidents including the 2001 anthrax attacks in the United States. Cleanup of contaminated sites is complex and costly.

Self-assessment MCQs (single best answer)
What bacterium causes anthrax?
What is the most common form of anthrax?
Which of the following is a characteristic symptom of cutaneous anthrax?
How can gastrointestinal anthrax be contracted?
Which antibiotic is commonly used to treat anthrax?
What is the function of monoclonal antibodies like raxibacumab in the treatment of anthrax?
Who first identified Bacillus anthracis?
What is the name of the FDA-approved anthrax vaccine?
Which part of the body does inhalation anthrax primarily affect?
What year did Louis Pasteur develop the first effective anthrax vaccine?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


