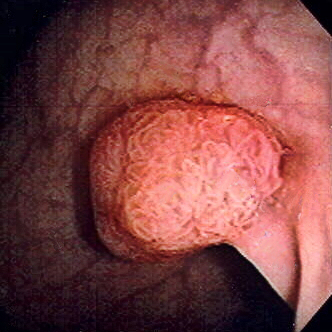
Colorectal Polyp
A colorectal polyp is a fleshy growth occurring on the lining of the colon or rectum. If left untreated, colorectal polyps can develop into colorectal cancer. They are often classified based on their behaviour (benign vs. malignant) or cause, such as inflammatory bowel disease.
Polyps can be benign (e.g., hyperplastic polyp), pre-malignant (e.g., tubular adenoma), or malignant (e.g., colorectal adenocarcinoma).
Signs and Symptoms
Colorectal polyps are typically asymptomatic. When symptoms do occur, they may include bloody stools, changes in stool frequency or consistency, and fatigue due to blood loss. Anaemia from iron deficiency can also present without visible blood in the stool. Increased mucus production, particularly with villous adenomas, can lead to symptomatic hypokalaemia. If a polyp is large enough, it can cause bowel obstruction, leading to nausea, vomiting, and severe constipation.
Structure
Polyps can be pedunculated (attached to the intestinal wall by a stalk) or sessile (growing directly from the wall). Histologically, they are divided into tubular adenomas (tubular glands), villous adenomas (finger-like projections), and tubulovillous adenomas (features of both).
Genetics
Hereditary syndromes associated with increased colorectal polyp formation include Familial Adenomatous Polyposis (FAP), Hereditary Nonpolyposis Colorectal Cancer (HNPCC or Lynch Syndrome), Peutz–Jeghers Syndrome, and Juvenile Polyposis Syndrome. Genes implicated in polyposis include GREM1, MSH3, MLH3, NTHL1, RNF43, and RPS20.
Familial Adenomatous Polyposis (FAP)
FAP involves the APC gene on chromosome q521 and presents with multiple polyps at an early age, all of which will eventually develop into cancer if untreated. The gene is autosomal dominant, with 10-20% of cases arising from spontaneous germline mutations. Colorectal cancer screening and surgical removal of affected tissues are recommended.
Hereditary Nonpolyposis Colorectal Cancer (HNPCC or Lynch Syndrome)
HNPCC is the most common hereditary form of colorectal cancer in the U.S., accounting for 3% of cases. It is characterised by early onset, proximal lesions, and a high response to surgical intervention. The condition is linked to dysfunctions in DNA repair mechanisms, involving genes such as hMSH2, hMSH1, hMSH6, and hPMS2.
Peutz–Jeghers Syndrome
This autosomal dominant syndrome presents with hamartomatous polyps and hyperpigmentation of the mouth, lips, and fingers. It is associated with the STK11 gene and increases the risk of both intestinal and extraintestinal cancers. Polyps larger than 1.5 cm require removal, and patients should be monitored closely.
Juvenile Polyposis Syndrome
Characterised by an increased risk of intestinal and extraintestinal cancers, this syndrome is linked to the SMAD4 gene. Multiple juvenile polyps increase the risk of malignancy, necessitating close monitoring and possibly surgical intervention.
Types
Colorectal polyps can be broadly classified into hyperplastic, neoplastic (adenomatous and malignant), hamartomatous, and inflammatory types.

Prevention
Diet and lifestyle significantly impact colorectal polyp formation. Protective factors include the consumption of cooked green vegetables, brown rice, legumes, and dried fruit.
Diagnosis
Colorectal polyps can be detected using various methods, including faecal occult blood tests, flexible sigmoidoscopy, colonoscopy, virtual colonoscopy, digital rectal examination, barium enema, or pill camera.
Treatment
Polyps can be removed during a colonoscopy or sigmoidoscopy using a wire loop that cuts and cauterises the stalk. Endoscopic mucosal resection (EMR) is used for larger, laterally spreading adenomas. Minimally invasive surgery is indicated for polyps too large or in unfavourable locations for endoscopic removal.
Follow-up
U.S. guidelines recommend follow-up intervals based on initial findings. For example, normal findings suggest a 10-year interval, while multiple adenomas or larger adenomas may necessitate more frequent monitoring.




Self-assessment MCQs (single best answer)
Which type of colorectal polyp is considered pre-malignant?
Which hereditary syndrome is associated with the APC gene on chromosome q521?
Which of the following is a typical symptom of colorectal polyps?
What type of polyp is characterised by finger-like projections?
Which diagnostic method involves the use of a wire loop to remove polyps?
Peutz–Jeghers Syndrome is associated with which gene?
Which type of colorectal polyp is generally benign?
In which hereditary syndrome do patients present with hamartomatous polyps and mucocutaneous hyperpigmentation?
Which gene is linked to Juvenile Polyposis Syndrome?
What is the recommended follow-up interval for normal findings in a colonoscopy?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


