Faecal Incontinence
Faecal incontinence (FI), or encopresis in some forms, is the involuntary loss of bowel contents, including liquid stool, mucus, or solid faeces. When flatus (gas) is also lost, it is referred to as anal incontinence. FI is a symptom rather than a diagnosis and can result from various causes, including childbirth damage, anorectal surgery complications, bowel habit changes, and neurological disorders.

Signs and Symptoms
FI significantly impacts individuals' physical and mental health, affecting personal, social, and professional life. Emotional effects include stress, anxiety, depression, and humiliation, while physical symptoms may involve skin soreness, pain, and odour. Physical activities, travel, and relationships are often affected.
Causes
FI results from a complex interplay of multiple factors, typically involving obstetric injury, anorectal surgery, neurological disorders, constipation/faecal loading, cognitive dysfunction, diarrhoea, and inflammatory bowel diseases. Specific causes in children may include anorectal anomalies and spinal cord defects.
Anal Canal
The anal canal's functioning can be affected by trauma or surgery, leading to incontinence. Obstetric injuries, such as sphincter tears during childbirth, are common causes. Nontraumatic conditions like scleroderma, nerve damage, and radiation therapy can also weaken the anal sphincters.
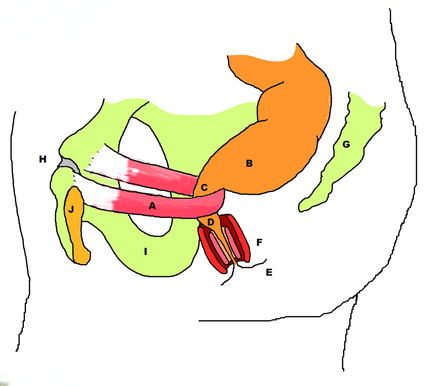
Pelvic Floor
Weakness of the pelvic floor, especially the puborectalis muscle, can contribute to FI. Recurrent straining and nerve damage during labour or constipation may lead to pelvic floor weakness and incontinence.
Rectum
Rectal storage capacity and sensation are very important for continence. Surgery, radiotherapy, inflammatory bowel disease, and tumours can impair rectal compliance and reservoir function, leading to urge incontinence or faecal loading and overflow FI.
Central Nervous System
Brain and spinal cord damage, such as stroke, tumours, multiple sclerosis, and dementia, can affect continence. Conditions like epilepsy may also cause FI during seizures.
Diarrhoea
Liquid stool is harder to control than solid stool, making diarrhoea a common aggravating factor. Chronic conditions like irritable bowel syndrome and Crohn's disease can cause prolonged diarrhoea and FI.
Overflow Incontinence
Large masses of faeces in the rectum can cause liquid stool to bypass the obstruction, leading to FI. Hospitalised patients and care home residents are particularly susceptible.

Diagnosis
Diagnosis involves a thorough medical history, digital rectal examination, and anorectal physiology tests. Tests like anorectal manometry, anal electromyography, and pudendal nerve terminal motor latency assess sphincter function and nerve damage. Proctography, proctosigmoidoscopy, and endoanal ultrasound help visualise structural defects and evaluate rectal storage capacity.
Management
FI management includes conservative measures, surgery, or a combination of both. Treatments are tailored to the underlying cause and severity. Conservative measures include dietary modification, pharmacological management, retrograde anal irrigation, biofeedback, and anal sphincter exercises.
Diet
Dietary modification addresses underlying causes like diarrhoea or constipation. Increasing dietary fibre and reducing certain foods and beverages can help manage symptoms.
Medication
Anti-diarrheal agents, laxatives, and stool bulking agents may be used. Cholestyramine can help those with bile acid diarrhoea post-gallbladder removal.
Other Measures
Evacuation aids, such as suppositories, enemas, and transanal irrigation, can help manage FI. Biofeedback and pelvic floor exercises aim to strengthen the pelvic floor muscles and improve continence.
Surgery
Surgical options are considered when conservative measures are insufficient. Procedures include sphincteroplasty, sacral nerve stimulation, dynamic graciloplasty, and faecal diversion. The choice of surgery depends on the specific cause and extent of sphincter damage.

Epidemiology
FI is common but often under-reported due to embarrassment. It affects people of all ages, with higher prevalence in older adults and females. Risk factors include age, female gender, urinary incontinence, vaginal delivery, obesity, and prior anorectal surgery.
History
Colonic irrigation was historically the primary treatment for FI. Surgical advancements began in the late 18th century, with sphincter repair techniques and biofeedback introduced in the mid-20th century. Recent developments include dynamic graciloplasty and sacral nerve stimulation.
Society and Culture
FI is a highly stigmatised condition, leading to social exclusion and reduced quality of life. Economic costs are significant, with high healthcare expenses and productivity losses. In some cultures, incontinence-related insults are common, highlighting the societal challenges faced by individuals with FI.
Self-assessment MCQs (single best answer)
What is faecal incontinence (FI)?
What is anal incontinence?
Which of the following is NOT a potential cause of faecal incontinence?
Which muscle's weakness can contribute to faecal incontinence?
Which diagnostic test is used to assess sphincter function and nerve damage in faecal incontinence?
Which of the following is a conservative measure for managing faecal incontinence?
What is the purpose of biofeedback in the management of faecal incontinence?
Which medication might be helpful for someone with bile acid diarrhoea post-gallbladder removal?
What is the historical primary treatment for faecal incontinence?
Which of the following is a common risk factor for faecal incontinence?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


