Fatty Liver Disease
Fatty liver disease (FLD), also known as hepatic steatosis, is a condition characterised by excessive fat accumulation in the liver. It can be asymptomatic or present with symptoms such as tiredness or pain in the upper right abdomen. Complications include cirrhosis, liver cancer, and oesophageal varices.
Classification
FLD is classified into two main subtypes:
- Metabolic dysfunction–associated steatotic liver disease (MASLD), formerly non-alcoholic fatty liver disease (NAFLD), which includes metabolic dysfunction-associated steatohepatitis (MASH).
- Alcohol-associated liver disease (ALD).
An overlap category, metabolic and alcohol associated liver disease (metALD), describes individuals with MASLD who consume significant amounts of alcohol but not enough to be categorised as ALD.
Signs and Symptoms
Most individuals with FLD are asymptomatic. When symptoms occur, they can include:
- Tiredness
- Pain in the upper right side of the abdomen
Complications
FLD can progress to hepatic fibrosis, cirrhosis, or liver cancer. The 10-year survival rate for NAFLD is around 80%. The progression of fibrosis varies, occurring faster in those with nonalcoholic steatohepatitis (NASH) compared to those with simple fatty liver. NASH can lead to hepatocellular carcinoma even without cirrhosis.
Causes
FLD is associated with metabolic syndrome (diabetes, hypertension, obesity, dyslipidaemia), alcohol use, certain medications, and other conditions such as hepatitis C and HIV.
Pathology
The disease process begins with the accumulation of triglycerides in hepatocytes. Initially, small fat vacuoles surround the nucleus (microvesicular fatty change). As the disease progresses, larger vacuoles displace the nucleus to the cell periphery, creating a signet ring appearance (macrovesicular fatty change). Macrovesicular steatosis is common in alcohol use, diabetes, obesity, and corticosteroid use.
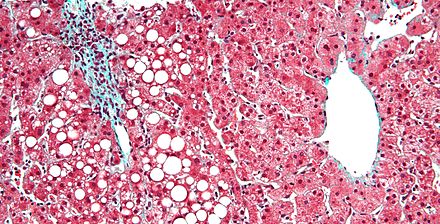
Severe fatty liver can lead to steatohepatitis, characterised by inflammation. Both alcoholic steatohepatitis (ASH) and non-alcoholic steatohepatitis (NASH) show similar pathological lesions. Hepatocyte ballooning, necrosis, and perisinusoidal fibrosis are common in advanced stages.

Diagnosis
Diagnosis involves medical history, blood tests, imaging, and occasionally liver biopsy. Elevated liver enzymes, particularly an AST:ALT ratio greater than 2:1 in alcoholic FLD and the reverse in nonalcoholic FLD, can be indicative. Imaging such as ultrasound, CT, and MRI can detect fatty infiltration.


Treatment
Treatment focuses on lifestyle changes, including dietary adjustments and exercise to induce weight loss. Medications that address insulin resistance and hyperlipidaemia, as well as bariatric surgery in severe cases, can improve or resolve the condition. In cases of drug-induced FLD, discontinuing the offending agent is essential.
Epidemiology
FLD is prevalent, affecting about 30% of people in Western countries and 10% in Asia. In the United States, it affects around 35% of the population, with 7% having NASH. Children in the US are also affected, with a 10% prevalence rate. The condition is more common in Hispanic populations compared to whites and blacks.

In Animals
FLD can occur in pets like reptiles, birds, and mammals, often due to overnutrition. In birds, a distinct sign is a misshapen beak. FLD can also be induced in geese or ducks for foie gras production and in ruminants like sheep through a high-calorie diet.
Self-assessment MCQs (single best answer)
What is another term for Fatty Liver Disease (FLD)?
What are the two main subtypes of FLD?
Which symptom is commonly associated with FLD?
What is the 10-year survival rate for non-alcoholic fatty liver disease (NAFLD)?
Which condition is not typically associated with FLD?
What is a common finding in the pathology of FLD?
What diagnostic ratio is indicative of alcoholic fatty liver disease (ALD)?
Which imaging modality is commonly used to detect fatty infiltration in the liver?
What is a primary focus in the treatment of FLD?
In which population is FLD more prevalent?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


