Hashimoto's Thyroiditis
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis or Hashimoto's disease, is an autoimmune disorder characterised by the gradual destruction of the thyroid gland. This condition often leads to hypothyroidism, where the thyroid gland fails to produce sufficient thyroid hormones, affecting various bodily functions.
Signs and Symptoms

In the early stages, symptoms may be subtle or unnoticed. Over time, the thyroid may enlarge, forming a painless goitre. Common symptoms include fatigue, weight gain, pale or puffy face, feeling cold, joint and muscle pain, constipation, dry and thinning hair, heavy menstrual flow or irregular periods, depression, and panic disorder.
In the advanced stages, the thyroid typically shrinks, potentially leading to hypothyroidism complications like high cholesterol, heart disease, heart failure, high blood pressure, and myxedema.

Diagnosis
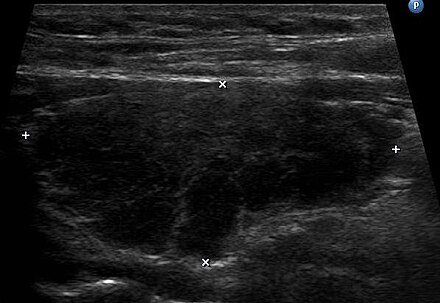
Diagnosis of Hashimoto's thyroiditis is confirmed through blood tests that measure thyroid-stimulating hormone (TSH), free T4, and the presence of antithyroid autoantibodies like anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin (anti-Tg). Ultrasound imaging of the thyroid can also be useful, especially in seronegative cases, by detecting characteristic features such as echogenicity, heterogeneity, hypervascularity, and the presence of small cysts.
Pathophysiology
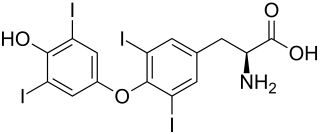
The mechanism behind Hashimoto's thyroiditis involves a complex interaction of genetic and environmental factors. The immune system mistakenly targets thyroid proteins, leading to inflammation and thyroid damage. This is marked by the presence of antibodies against thyroid peroxidase (TPOAb) and thyroglobulin (TgAb).
Histologically, the thyroid shows parenchymal infiltration by lymphocytes and plasma cells, with fibrotic tissue and atrophy in advanced stages.

Treatment
The primary treatment for Hashimoto's thyroiditis is thyroid hormone replacement therapy to manage hypothyroidism. Levothyroxine is the standard medication, dosed based on weight or TSH levels. The goal is to normalise thyroid hormone levels, which usually requires lifelong treatment. In some cases, combination therapy with levothyroxine and liothyronine (synthetic T3) is considered.
Regular monitoring of TSH levels is essential to ensure effective management, with adjustments made based on the patient's response.
Surgery Considerations
Surgery is rarely required and is generally reserved for patients with significant symptoms such as pressure effects, cosmetic concerns, or the presence of nodules. In severe cases, total thyroidectomy may be considered, which has been shown to resolve symptoms but comes with potential complications.
Prognosis
Patients with Hashimoto's thyroiditis have a risk of developing overt thyroid dysfunction, with about 5% progressing to thyroid failure annually. Rare complications include thyroid lymphoma and severe fibrous autoimmune thyroiditis, which may present with symptoms resembling aggressive thyroid tumours. Transient thyrotoxicosis can also occur due to inflammation-induced thyroid damage.
Epidemiology
Hashimoto's thyroiditis is the most common cause of hypothyroidism in iodine-sufficient regions. It affects approximately 2% of the global population and is more prevalent in women, with a female-to-male ratio of about 10:1. The incidence peaks between ages 30 and 50. High iodine intake, genetic predisposition, and the presence of other autoimmune diseases are significant risk factors.

Pregnancy
Pregnant women with Hashimoto's need careful monitoring and management to avoid complications such as miscarriage, preterm delivery, and neonatal issues. Thyroid function should be stabilised, and thyroid peroxidase antibodies (TPOAb) testing is recommended for all pregnant women to assess risk. Close cooperation between endocrinologists and obstetricians is very important for optimal maternal and foetal outcomes.
Self-assessment MCQs (single best answer)
What is another name for Hashimoto's thyroiditis?
Which of the following is NOT a common symptom of Hashimoto's thyroiditis?
Which blood test is used to confirm the presence of Hashimoto's thyroiditis?
What type of imaging can be useful in diagnosing Hashimoto's thyroiditis?
Which histological feature is characteristic of advanced Hashimoto's thyroiditis?
What is the standard medication for treating hypothyroidism due to Hashimoto's thyroiditis?
How often do patients with Hashimoto's thyroiditis typically need to monitor their TSH levels?
What is the female-to-male ratio for the prevalence of Hashimoto's thyroiditis?
Which of the following is a rare complication of Hashimoto's thyroiditis?
What is an important consideration for pregnant women with Hashimoto's thyroiditis?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


