Hepatoblastoma
Hepatoblastoma is a malignant liver cancer that primarily affects infants and children. It is composed of tissue resembling foetal liver cells, mature liver cells, or bile duct cells. The disease typically presents with an abdominal mass and is most commonly diagnosed during a child's first three years of life. Elevated alpha-fetoprotein (AFP) levels are a common diagnostic marker; however, the prognosis is poorer when AFP levels are not elevated at diagnosis.

Overview
Patients with hepatoblastoma are usually asymptomatic at the time of diagnosis, which often leads to the disease being advanced by the time it is detected. The most noticeable sign is typically an abdominal mass, which is often the first indication that prompts further investigation.
Signs and Symptoms
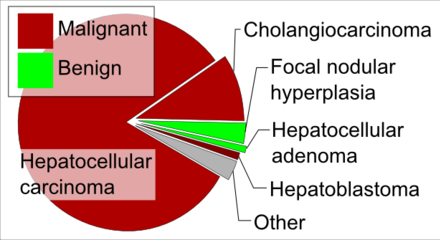
Hepatoblastomas originate from immature liver precursor cells and are typically unifocal, affecting the right lobe of the liver more frequently than the left. These tumours can metastasize. Hepatoblastomas are categorised into two types: "Epithelial Type" and "Mixed Epithelial / Mesenchymal Type."

Certain genetic conditions and syndromes are associated with an increased incidence of hepatoblastoma. For instance, individuals with familial adenomatous polyposis (FAP) frequently develop hepatoblastomas. Beta-catenin mutations are common in sporadic hepatoblastomas, occurring in up to 67% of patients. Other syndromes with increased hepatoblastoma incidence include Beckwith–Wiedemann syndrome, trisomy 18, trisomy 21, Acardi syndrome, Li–Fraumeni syndrome, Goldenhar syndrome, von Gierke disease, and familial adenomatous polyposis.
Diagnosis
The primary diagnostic method for hepatoblastoma is a blood test to check AFP levels. AFP serves as a biomarker to determine the presence of liver cancer in children. At birth, infants have high AFP levels, which fall to normal adult levels by the second year of life. Normal AFP levels are considered to be lower than 50 nanograms per millilitre (ng/ml) in children and 10 ng/ml in adults. An AFP level greater than 500 ng/ml is a significant indicator of hepatoblastoma. AFP levels are also monitored to assess treatment efficacy, with expected normalisation of AFP levels if treatments are successful.
Treatment
Treatment options for hepatoblastoma include surgical removal of the tumour, neoadjuvant chemotherapy prior to surgery, and liver transplantation. Primary liver transplantation offers a high long-term disease-free survival rate of approximately 80%. In cases where complete tumour removal and adjuvant chemotherapy are achieved, survival rates can approach 100%. The presence of metastases is the strongest predictor of poor prognosis.
Self-assessment MCQs (single best answer)
What is hepatoblastoma primarily composed of?
At what age is hepatoblastoma most commonly diagnosed?
Which biomarker is commonly elevated in patients with hepatoblastoma?
What is the most noticeable sign of hepatoblastoma?
Which genetic condition is frequently associated with hepatoblastomas?
Hepatoblastomas are categorised into which two types?
Which of the following is NOT a syndrome associated with increased hepatoblastoma incidence?
What AFP level is considered a significant indicator of hepatoblastoma?
What is the strongest predictor of poor prognosis in hepatoblastoma?
Which treatment option offers a high long-term disease-free survival rate of approximately 80% for hepatoblastoma?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


