Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a group of inflammatory conditions affecting the colon and small intestine, primarily comprising Crohn's disease and ulcerative colitis (UC). Crohn's disease can impact any part of the gastrointestinal tract from the mouth to the anus, while UC is typically confined to the colon and rectum.
IBD is a complex condition resulting from the interaction of environmental and genetic factors leading to immunological responses and intestinal inflammation.
Signs and Symptoms
Common symptoms of both Crohn's disease and UC include abdominal pain, diarrhoea, rectal bleeding, severe cramps, and weight loss. Unique symptoms for Crohn's disease include porridge-like defecation, less common tenesmus, common fistulae, and frequent weight loss.
In UC, symptoms include mucus-like defecation often with blood, more common tenesmus, severe fever, and seldom fistulae. Extraintestinal manifestations include arthritis, pyoderma gangrenosum, primary sclerosing cholangitis, and non-thyroidal illness syndrome.
Diagnostic Findings
Crohn's Disease
- Common terminal ileum involvement
- Patchy areas of inflammation (skip lesions)
- Deep geographic and serpiginous ulcers
- Transmural inflammation
- Common stenosis and non-necrotising granulomas
Ulcerative Colitis
- Continuous inflammation always involving the colon
- Shallow, mucosal ulcers
- Higher rate of primary sclerosing cholangitis
- Continuous area of inflammation without skip lesions
Causes
Diet
Diet plays a role in managing IBD. Diets high in fruits, vegetables, and water while low in processed meats and refined carbohydrates are associated with a lower risk of active symptoms.
Gluten sensitivity is common in IBD, potentially leading to flare-ups. High intake of animal protein and sugar may increase IBD risk and relapses.
Bile Acids
IBD patients exhibit an increased abundance of primary bile acids and a decreased abundance of secondary bile acids, indicating their potential role in IBD pathogenesis.
Microbiota
IBD is associated with a dysbiotic microbiota, characterised by reduced beneficial bacteria and increased harmful species. Oxidative stress and a breach of the intestinal barrier contribute to IBD pathophysiology, with an exaggerated immune response causing further epithelial damage.
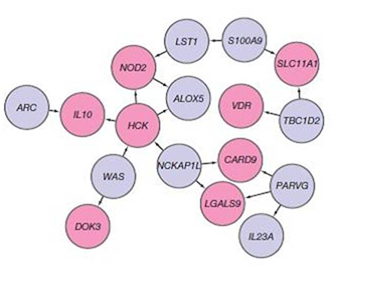
Genetics
IBD has a significant genetic component. Over 200 SNPs are linked to IBD susceptibility.
Genetic studies reveal that mutations in IBD-associated genes may disrupt normal immune responses, contributing to disease development.
Diagnosis
Diagnosis involves stool inflammatory markers and colonoscopy with biopsy. Faecal calprotectin is a useful initial test.
IBD classification distinguishes between Crohn's disease and UC based on the location and nature of inflammation. While Crohn's disease can affect any part of the GI tract with skip lesions, UC is restricted to the colon and rectum with continuous mucosal inflammation.
Treatment
Medical Therapies
Treatment is individualised, often starting with anti-inflammatory drugs like prednisone. Maintenance therapy may include mesalazine for UC, while Crohn's may require immunosuppressants like azathioprine.
Biological therapies, including TNF inhibitors, are used for severe or resistant cases.
Surgery
UC can often be cured by proctocolectomy, while Crohn's disease may require surgery for complications but cannot be cured. Surgical interventions include bowel resection and creating stomas for waste collection.
Nutritional and Dietetic Therapies
Nutritional deficiencies are common in IBD. Exclusive enteral nutrition is a first-line therapy in paediatric Crohn's disease.
Dietary fibre interventions and specific exclusion diets can help manage symptoms. Vitamin and mineral supplementation is very important for addressing deficiencies.
Microbiome and Alternative Therapies
Antibiotic and probiotic therapies are looked at for modifying the gut microbiome. Faecal microbiota transplant shows variable efficacy.
Herbal therapies, mind/body interventions, and acupuncture have supportive evidence for symptom management.
Novel Approaches
Stem cell therapy shows promise but is not yet standard. Psychological interventions may benefit adolescents but require more research for adults.
Prognosis
Complications like nutrient deficiency, colon cancer, and extraintestinal manifestations are concerns. While IBD is rarely fatal, it significantly affects quality of life.
Routine surveillance for colorectal cancer and managing flare-ups are essential aspects of patient care.
Self-assessment MCQs (single best answer)
Which of the following is a characteristic finding in Crohn's disease but not typically in ulcerative colitis?
Which type of diet is associated with a lower risk of active symptoms in patients with IBD?
What is the most common extraintestinal complication of inflammatory bowel disease?
Which diagnostic test is initially useful in suggesting the possibility of IBD due to its sensitivity?
Which of the following is a first-line therapy in paediatric Crohn's disease?
In IBD patients, which of the following is more commonly seen in Crohn's disease compared to ulcerative colitis?
Which genetic factor was the first to be linked to IBD?
What surgical procedure is most often curative for ulcerative colitis?
Which probiotic-related treatment has shown variable efficacy in IBD but is considered safe?
Which of the following complications is more commonly associated with ulcerative colitis than with Crohn's disease?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


