Interstitial Lung Disease (ILD)
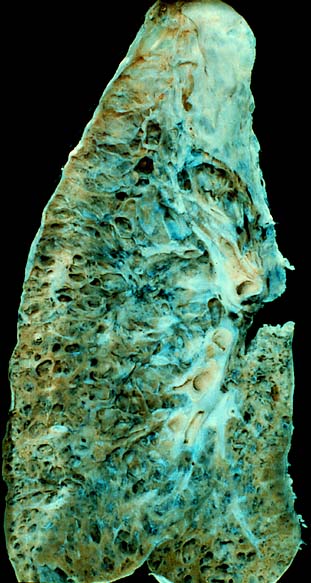
Interstitial lung disease (ILD), also referred to as diffuse parenchymal lung disease (DPLD), is a group of respiratory conditions that primarily affect the interstitium, which includes the tissue and space around the alveoli (air sacs) of the lungs.
This disease affects the alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues.
When an injury to the lungs prompts an abnormal healing response, the tissue around the alveoli becomes scarred and thickened, making oxygen transfer to the bloodstream more difficult.
Signs & Symptoms
The symptoms of ILD develop gradually over several months and include shortness of breath, nonproductive coughing, fatigue, and weight loss. Thirty to 40% of those with ILD eventually develop pulmonary fibrosis, which has a median survival of 2.5-3.5 years. The average survival rate for ILD patients is between three and five years.

Causes
ILD can be classified based on whether the cause is unknown (idiopathic) or known (secondary). Idiopathic interstitial pneumonia represents the majority of ILD cases, with subtypes such as idiopathic pulmonary fibrosis (IPF), desquamative interstitial pneumonia (DIP), and acute interstitial pneumonia (AIP). Secondary ILDs have known etiologies, including connective tissue and autoimmune diseases, inhaled substances, drug-induced reactions, infections, and malignancies.

Diagnosis
Diagnosis involves assessing clinical signs and symptoms, occupational exposures, and imaging studies. ILD usually presents with dyspnea and chronic cough. Velcro crackles are common on examination. Pulmonary function tests typically show a restrictive defect with decreased diffusion capacity of carbon monoxide (DLCO). Chest X-rays and high-resolution CT scans are essential in diagnosis, with CT scans being more sensitive and specific. Lung biopsies, including video-assisted thoracoscopic surgery (VATS) and bronchoscopic transbronchial cryobiopsy, may be required when imaging is inconclusive.


Pulmonary Function Testing
Pulmonary function tests are very important for diagnosis and assessing disease severity. Most ILDs follow a restrictive pattern, characterised by decreased TLC, RV, FVC, and FEV1. As the disease progresses, these values further decrease, indicating more severe disease and poorer prognosis.
Imaging
Chest radiography is often the first test, but high-resolution CT (HRCT) is preferred for its greater resolution. Radiologic appearance alone is insufficient and must be interpreted in the clinical context. ILD can be classified by patterns of opacities (consolidation, linear or reticular opacities, small nodules, cystic airspaces, ground glass opacities) and distribution (upper lung, lower lung, central, peripheral).
Genetic Testing
Genetic testing can identify specific mutations in paediatric ILDs and some adult ILDs, offering a precise molecular diagnosis without the need for lung biopsy.
Treatment
Treatment varies based on the specific type of ILD. Avoidance of identified occupational or drug causes is essential. Oxygen therapy improves quality of life, though its impact on mortality is uncertain. Pulmonary rehabilitation enhances exercise capacity and quality of life. Lung transplantation is an option for progressive ILD, with a median survival of 5.2 years post-transplant for idiopathic interstitial pneumonias.
Medications
Antifibrotics such as pirfenidone and nintedanib slow lung function decline. Immunomodulators like tocilizumab, cyclophosphamide, mycophenolate mofetil, and rituximab improve lung function in specific ILD subtypes. Treprostinil, an inhaled vasodilator, improves exercise capacity in pulmonary hypertension secondary to ILD.
Supportive Care
Supportive measures include smoking cessation, vaccinations, and short-acting opiates for breathlessness and cough management.

Self-assessment MCQs (single best answer)
Which part of the lungs is primarily affected by Interstitial Lung Disease (ILD)?
Which of the following is NOT a common symptom of ILD?
What is the median survival range for patients with pulmonary fibrosis?
Which diagnostic method is considered more sensitive and specific for ILD?
Which pulmonary function test value is typically decreased in ILD patients?
Which medication is classified as an antifibrotic used to treat ILD?
What is the role of oxygen therapy in ILD treatment?
Which of the following is NOT a potential cause of secondary ILD?
What is the median survival after lung transplantation for idiopathic interstitial pneumonias?
Which of the following supportive measures is recommended for ILD patients?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


