Meningitis
Meningitis is an acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges.
It is a serious medical emergency due to its proximity to the brain and spinal cord. The inflammation can be caused by infections with viruses, bacteria, fungi, or parasites, and non-infectious causes such as cancer and certain drugs.

Signs and Symptoms
In adults, the most common symptom of meningitis is a severe headache, followed by neck stiffness and fever.
The classic triad of meningitis includes neck stiffness, sudden high fever, and altered mental status, but all three are present in only 44–46% of cases. Other symptoms include photophobia and phonophobia. Small children may show nonspecific symptoms such as irritability, drowsiness, or poor feeding.

Meningitis caused by Neisseria meningitidis often features a rapidly spreading petechial rash, which is non-blanching and may precede other symptoms.
Causes
Bacterial
The causative bacteria vary by age group. In newborns, group B streptococci, E. coli, and Listeria monocytogenes are common. In older children and adults, Neisseria meningitidis and Streptococcus pneumoniae are prevalent. Bacterial meningitis can also occur from head injuries, cerebral shunts, or other devices in the brain.

Viral
Viral meningitis is usually caused by enteroviruses, herpes simplex virus, varicella zoster virus, mumps virus, and HIV. Viral meningitis is more common and generally less severe than bacterial meningitis.
Fungal and Parasitic
Cryptococcal meningitis is the most common fungal form, often affecting immunocompromised individuals. Parasitic meningitis can be caused by parasitic worms or amoebae, and is less common.
Non-Infectious
Non-infectious causes include malignancies, certain drugs, and inflammatory conditions like sarcoidosis and lupus.
Diagnosis
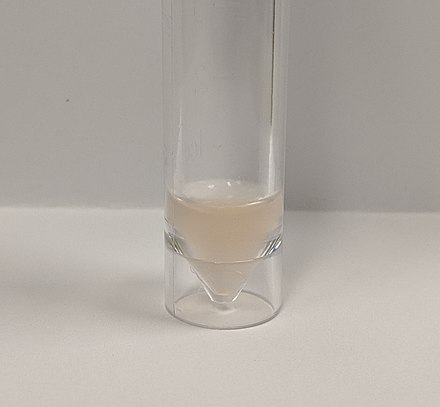
A lumbar puncture, or spinal tap, is essential for diagnosing meningitis. CSF analysis can reveal the presence and type of meningitis. CT or MRI scans may be required before lumbar puncture if there is a risk of raised intracranial pressure.

Treatment
Bacterial Meningitis
Immediate empiric antibiotic treatment is very important. The choice of antibiotics depends on age, preceding head injury, and immune status. Common antibiotics include third-generation cefalosporins like cefotaxime or ceftriaxone, sometimes combined with vancomycin or ampicillin.

Corticosteroids like dexamethasone are often used to reduce inflammation, particularly in cases of pneumococcal meningitis. Fluid therapy is essential for maintaining hydration and blood pressure.
Viral Meningitis
Treatment is mainly supportive, as most viruses cannot be targeted by specific medications. Herpes simplex and varicella zoster viruses may respond to antiviral drugs like aciclovir.
Fungal Meningitis
Fungal meningitis requires long courses of high-dose antifungals such as amphotericin B and flucytosine. Frequent lumbar punctures may be needed to relieve raised intracranial pressure.
Prevention
Vaccination
Vaccines are available for some forms of bacterial meningitis, including Haemophilus influenzae type B, meningococcal, and pneumococcal vaccines. These have significantly reduced the incidence of meningitis in vaccinated populations.
Antibiotics
Prophylactic antibiotics may be used in close contacts of people with meningococcal meningitis to reduce the risk of infection.
Prognosis
The prognosis of meningitis varies widely. Untreated bacterial meningitis is almost always fatal, but with treatment, the risk of death is reduced to less than 15% for bacterial forms. Viral meningitis generally resolves spontaneously and is rarely fatal. Long-term complications can include hearing loss, cognitive deficits, and epilepsy.

Self-assessment MCQs (single best answer)
Which of the following is NOT a common symptom of meningitis in adults?
What is the classic triad of symptoms for meningitis?
Which bacterium is a common cause of meningitis in newborns?
Which imaging technique might be required before a lumbar puncture if there is a risk of raised intracranial pressure?
What is the primary treatment for bacterial meningitis?
Which virus is NOT commonly associated with viral meningitis?
What is the most common fungal form of meningitis?
Which of the following is NOT a method for preventing bacterial meningitis?
Which drug is commonly used to reduce inflammation in cases of pneumococcal meningitis?
What is the typical prognosis for untreated bacterial meningitis?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


