Narcolepsy
Narcolepsy is a chronic neurological disorder affecting the regulation of sleep-wake cycles, particularly impacting REM (rapid eye movement) sleep. It is characterised by excessive daytime sleepiness (EDS), sleep-related hallucinations, sleep paralysis, disturbed nocturnal sleep (DNS), and cataplexy.
Narcolepsy is divided into two types: type 1 (NT1), which involves cataplexy and low levels of CSF orexin, and type 2 (NT2), which does not involve cataplexy and has normal CSF orexin levels.
Overview
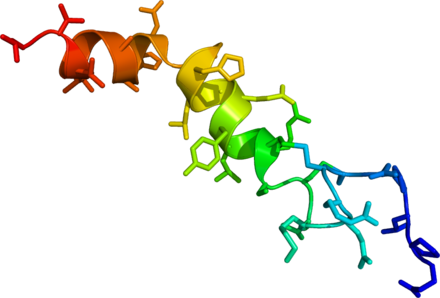
The concentration of orexin-A neuropeptides in the cerebrospinal fluid of narcoleptic individuals is usually very low.
Causes
The exact cause of narcolepsy is unknown, but it is linked to the loss of orexin-releasing neurons in the hypothalamus. This loss, typically involving about 70,000 neurons, disrupts the regulation of wakefulness and REM sleep. Genetic factors play a significant role, particularly variations in HLA genes that may trigger an autoimmune response against orexin-releasing neurons.
Environmental factors such as infections, especially H1N1 influenza, brain injuries, and exposure to toxins may also contribute.
Signs and Symptoms
Excessive Daytime Sleepiness (EDS)
EDS is a hallmark of narcolepsy and occurs even after adequate night-time sleep. Patients experience an overwhelming urge to sleep during the day, often resulting in unintended naps. These naps can be refreshing but only temporarily.
Cataplexy
Cataplexy involves sudden muscle weakness triggered by strong emotions like laughter or anger. It ranges from mild (e.g., drooping eyelids) to severe (e.g., complete body collapse) but the person remains conscious throughout.
Abnormal REM Sleep
Narcoleptics enter REM sleep almost immediately after falling asleep, unlike non-narcoleptics who typically enter REM after a period of non-REM sleep. This can lead to vivid dreams and hallucinations.
Sleep Paralysis and Hallucinations
Sleep paralysis is the temporary inability to move or speak while falling asleep or waking up. Hypnagogic (falling asleep) and hypnopompic (waking up) hallucinations are vivid and often frightening experiences.
Diagnosis
Diagnosis is based on symptoms and sleep studies, primarily polysomnography (PSG) and the Multiple Sleep Latency Test (MSLT). PSG records brain waves and muscle activity during night-time sleep, while MSLT measures how quickly a person falls asleep in a quiet environment during the day. Cerebrospinal fluid (CSF) analysis for orexin levels can provide conclusive evidence, especially for NT1.
Treatment
Behavioural Strategies
Patients benefit from lifestyle changes such as maintaining a regular sleep schedule, scheduled naps, and avoiding sleep-inducing foods. Social support and education about the condition are also very important.
Medications
Medications target EDS and cataplexy. They include alerting agents like modafinil, armodafinil, and pitolisant, which improve wakefulness. Sodium oxybate is effective for both EDS and cataplexy and is taken at night. Traditional stimulants like methylphenidate and amphetamines are also used. Antidepressants such as tricyclic antidepressants, SSRIs, and SNRIs are prescribed primarily for cataplexy.
New Treatments
Research is ongoing for treatments like hypocretin replacement therapies and gene editing. Hypocretin agonists and cell transplantation are potential future treatments.
Epidemiology
Narcolepsy affects approximately 1 per 2,000 people in the United States, with varying prevalence across different countries. It commonly begins in adolescence or young adulthood and affects both males and females equally. Misdiagnosis is common, often mistaken for depression, epilepsy, or other sleep disorders.
Research
Current research focuses on understanding the role of orexin and developing new treatments. Studies are looking at GABA-directed medications like flumazenil and clarithromycin, which show promise in counteracting excessive sleepiness. Orexin receptor agonists are also being investigated for their potential to regulate wakefulness effectively.
Narcolepsy remains a challenging disorder, but ongoing research and improved diagnostic methods offer hope for better management and treatment options.
Self-assessment MCQs (single best answer)
What is the primary characteristic of narcolepsy?
Which neuropeptide is typically low in the cerebrospinal fluid of individuals with narcolepsy type 1 (NT1)?
What is cataplexy triggered by?
Narcolepsy is divided into how many types?
Which diagnostic test measures how quickly a person falls asleep in a quiet environment during the day?
Which treatment is effective for both Excessive Daytime Sleepiness (EDS) and cataplexy in narcoleptic patients?
What is the prevalence of narcolepsy in the United States?
Which of the following is a potential future treatment for narcolepsy being researched?
Which symptom involves vivid and often frightening experiences while falling asleep or waking up?
What percentage of orexin-releasing neurons are typically lost in individuals with narcolepsy?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


