Pancreatic Cancer
Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply uncontrollably and form a mass. These cancerous cells can invade other parts of the body. The most common type, pancreatic adenocarcinoma, accounts for about 90% of cases. Other types include pancreatic neuroendocrine tumours (PanNETs), which are generally less aggressive.

Signs and Symptoms
Pancreatic cancer typically does not cause symptoms in its early stages. The most common form, pancreatic adenocarcinoma, may present symptoms like yellow skin (jaundice), abdominal or back pain, unexplained weight loss, light-coloured stools, dark urine, and loss of appetite. A significant number of patients have diabetes at the time of diagnosis, which may indicate the presence of a tumour.

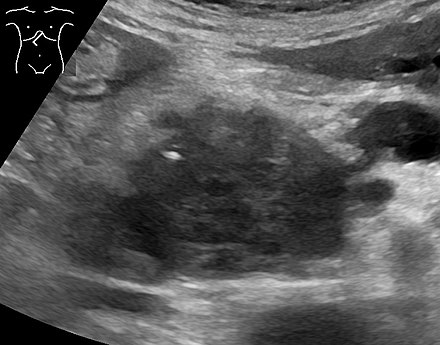
Diagnosis
Pancreatic cancer is usually diagnosed using a combination of medical imaging techniques like computed tomography (CT), endoscopic ultrasound (EUS), magnetic resonance imaging (MRI), and positron emission tomography (PET). Blood tests, liver function tests, and tumour markers such as CA19-9 may also be used. Biopsies by fine needle aspiration can confirm diagnosis.

Treatment
Treatment depends on the stage of the cancer. Surgery is the only potentially curative treatment and is possible in about 20% of cases. Various surgical procedures, like the Whipple procedure, are used depending on the tumour's location. Chemotherapy and radiotherapy are often used in conjunction with surgery or as palliative treatments to extend life and improve quality of life.

Surgery
Surgical options include the Whipple procedure, distal pancreatectomy, and palliative surgeries to bypass obstructions caused by the tumour. Despite advancements, surgery often comes with significant risks and complications.
Chemotherapy
Chemotherapy, including regimens like FOLFIRINOX and gemcitabine with nab-paclitaxel, is used to treat pancreatic cancer. These treatments can extend survival but come with substantial side effects. Neoadjuvant chemotherapy may be administered to shrink tumours before surgery.
Radiotherapy
Radiotherapy's role remains controversial but may be used to shrink tumours to a resectable size or as palliative care to manage symptoms.
Palliative Care
Palliative care focuses on symptom management and improving the quality of life. This includes managing pain with medications or nerve blocks, treating digestive issues with pancreatic enzyme supplements, and addressing psychological issues such as depression.
Prognosis
Pancreatic cancer generally has a poor prognosis, with a five-year survival rate of about 13%. However, early-stage cancers have better outcomes. PanNETs generally have a better prognosis, with a five-year survival rate of 65% for certain types.

Distribution
Pancreatic cancer is more common in developed countries and slightly more common in men. The disease's incidence increases with age, and it is notably more common in African Americans in the United States than in other ethnic groups.
Research Directions
Research is ongoing into genetics, early detection, surgical strategies, and targeted therapies. Trials are looking at novel adjuvant therapies, immunotherapy, and the use of nanoparticles to deliver drugs specifically to cancer cells, minimising side effects.

Self-assessment MCQs (single best answer)
What is the most common type of pancreatic cancer?
Which symptom is commonly associated with pancreatic adenocarcinoma?
What imaging technique is NOT typically used to diagnose pancreatic cancer?
What is the five-year survival rate for pancreatic cancer?
Which surgical procedure is commonly performed for tumours located in the head of the pancreas?
Which chemotherapy regimen is mentioned as a treatment for pancreatic cancer?
What role does radiotherapy primarily play in the treatment of pancreatic cancer?
Which of the following is a common complication of advanced pancreatic cancer?
Which tumour marker may be used in the diagnosis of pancreatic cancer?
What is the main focus of palliative care in pancreatic cancer patients?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


