Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome (PFPS), also known as patellar overload syndrome, runner's knee, or retropatellar pain syndrome, is a medical condition causing pain in the front of the knee due to issues between the kneecap and the femur. This condition is particularly common among runners and young adults, occurring more frequently in females than males.

Signs and Symptoms
PFPS generally has a gradual onset, although some cases may appear suddenly following trauma. The most common symptom is diffuse, vague pain around the kneecap (peripatellar) and localised pain behind the kneecap (retropatellar). Individuals often have difficulty pinpointing the exact location of the pain, often describing it with a "circle sign" around the patella. Pain is typically initiated with activities that load the knee extensor mechanism, such as ascending or descending stairs, squatting, kneeling, cycling, or running. Prolonged sitting, sometimes termed the "movie sign" or "theatre sign," can also exacerbate the pain. The pain is usually aching and occasionally sharp, and may be accompanied by knee joint noises such as clicking, though these sounds are not related to pain and function. Some may report a sensation of the knee giving way and reduced knee flexion during activities.
Causes
The exact cause of PFPS is unclear, but it is believed to be due to overuse and increased pressure on the patellofemoral joint. Common contributing factors include trauma, increased levels of physical activity, malalignment of the patella, quadriceps muscle imbalance, and tight anatomical structures such as the retinaculum or iliotibial band. Excessively worn or poorly fitted footwear may also contribute. Preventing recurrence involves identifying and managing these causal factors correctly.
Diagnosis
Examination
Diagnosis is primarily based on symptoms and physical examination. Observations of patellar alignment during standing and walking, along with tests such as the Q-angle, lateral hypermobility, and J-sign, can help determine patellar maltracking. The patellofemoral grind test (Clarke's sign) and the patellar apprehension test are commonly used to provide evidence for PFPS. MRI is rarely useful except in cases with mechanical symptoms like a locked knee or failure to improve following physical therapy.
Differential Diagnosis
PFPS must be differentiated from conditions such as patellar tendinitis, prepatellar bursitis, plica syndrome, Sinding-Larsen and Johansson syndrome, and Osgood–Schlatter disease. Currently, there is no gold standard assessment for diagnosing PFPS.
Treatment
Exercises
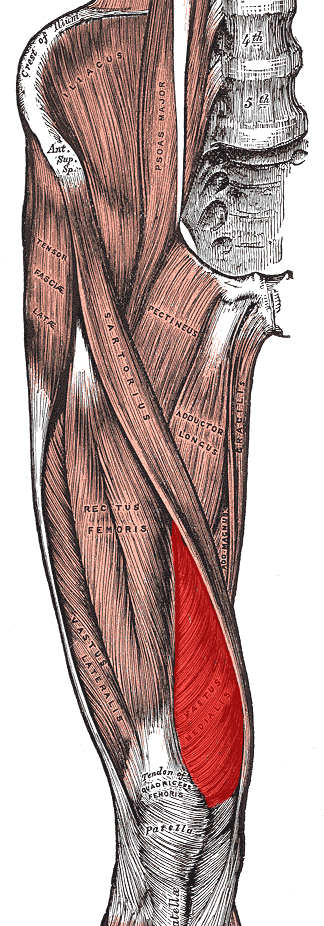
Exercise therapy is the recommended first-line treatment, focusing on reducing knee activity until the pain resolves. Exercises typically aim to strengthen the quadriceps muscles to address muscle imbalance and improve patellar tracking. Additionally, hip abductor, extensor, and external rotator strengthening may help. Stretches to improve lower limb flexibility are often included. Electromyographic biofeedback may assist individuals in targeting specific muscles during exercises.
Manual Therapy
Manual therapy in conjunction with exercises can reduce pain and improve function. Techniques such as patellar joint mobilisation and soft tissue mobilisation are effective, though there is limited evidence supporting lumbopelvic spine manipulation.
Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat PFPS, but evidence of their long-term effectiveness is limited.
Braces and Taping
Taping may help reduce pain when combined with therapeutic exercises, although knee braces are generally ineffective in treating PFPS.
Insoles
Foot orthoses can help improve lower extremity biomechanics and may be useful in reducing knee pain in the short term, though there is no evidence supporting their long-term use.
Surgery
Surgery is generally avoided except in severe cases where conservative treatments fail.
Alternative Medicine
There is no substantial evidence supporting the use of alternative therapies such as acupuncture or low-level laser therapy for PFPS.
Prognosis
PFPS can become a chronic condition, with around 50% of individuals reporting persistent pain after a year. Factors such as age, sex, body weight, and muscle strength can influence recovery duration.
Epidemiology
PFPS is the most common cause of anterior knee pain, particularly in populations such as runners, bicyclists, basketball players, young athletes, and females. While BMI does not significantly increase the risk in adolescents, higher BMI in adults is associated with limited physical activity due to pain.
Self-assessment MCQs (single best answer)
Which of the following is NOT a common symptom of Patellofemoral Pain Syndrome (PFPS)?
What is another term used to describe PFPS?
Which of the following tests is commonly used in diagnosing PFPS?
Which muscle is often targeted in exercise therapy for PFPS?
Which of the following is NOT a commonly identified cause of PFPS?
Which treatment is generally ineffective in treating PFPS?
Which of the following is NOT a typical activity that exacerbates PFPS pain?
In terms of epidemiology, which group is more frequently affected by PFPS?
What is the prognosis for individuals with PFPS?
Which of the following does NOT contribute to the development of PFPS?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


