Peutz–Jeghers Syndrome
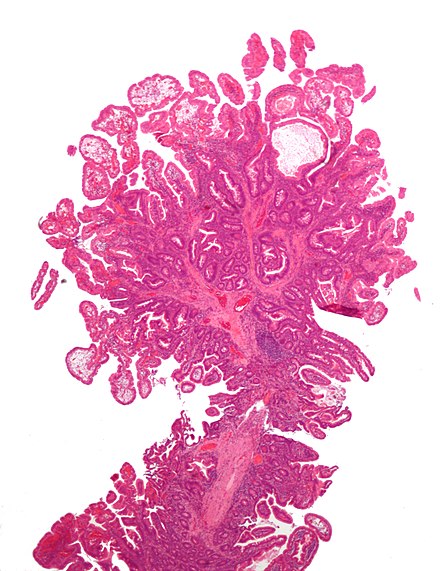
Peutz–Jeghers syndrome (PJS) is an autosomal dominant genetic disorder characterised by the development of benign hamartomatous polyps in the gastrointestinal tract and hyperpigmented macules on the lips and oral mucosa (melanosis).
This syndrome falls under hereditary intestinal polyposis and hamartomatous polyposis syndromes. It has an incidence of approximately 1 in 25,000 to 300,000 births.

Signs and Symptoms
Patients with Peutz–Jeghers syndrome have a substantial risk of cancer, particularly in the breast and gastrointestinal tracts. Colorectal cancer is the most common malignancy, with a lifetime risk of 39%, followed by breast cancer in females with a lifetime risk of 32 to 54%. There is also an increased risk of developing cancers of the liver, lungs, ovaries, uterus, testes, and other organs. Specifically, there is a heightened risk of sex-cord stromal tumours with annular tubules in the ovaries.
Due to these risks, direct surveillance is recommended. The average age of first diagnosis is 23, often presenting initially as bowel obstruction or intussusception from hamartomatous gastrointestinal polyps. Dark blue, brown, and black pigmented mucocutaneous macules are present in over 95% of individuals with PJS. These macules typically appear before the age of 5 and may fade during puberty. Though the macules are not associated with malignant transformation, complications such as obstruction and intussusception can occur in up to 69% of patients, often between the ages of 6 and 18. Anaemia due to gastrointestinal bleeding from the polyps is also common.
Genetics
The genetic mutation associated with PJS was identified in 1998. On chromosome 19, the gene known as STK11 (LKB1) is a possible tumour suppressor gene. PJS is inherited in an autosomal dominant pattern, meaning there is a 50% chance of passing the condition on to offspring. Despite being rare, PJS studies often include only a small number of patients, leading to variability in cancer risk estimates. There is an estimated 18–21% risk of ovarian cancer, 9% risk of endometrial cancer, and 10% risk of cervical cancer, particularly adenoma malignum.
Diagnosis

The main criteria for clinical diagnosis include a family history of PJS, mucocutaneous lesions causing hyperpigmentation in the mouth and on the hands and feet, and hamartomatous polyps in the gastrointestinal tract. Oral pigmentations are often the first to appear and play a very important role in early diagnosis. These are most frequently seen on the gingiva, hard palate, and inside the cheek, with the lower lip mucosa almost invariably involved. Having two of the three listed clinical criteria indicates a positive diagnosis. Molecular genetic testing for mutations in the STK11/LKB1 gene is available clinically.
Management
Resection of polyps is necessary only if serious bleeding or intussusception occurs. Enterotomy is performed to remove large, single nodules, and short lengths of heavily involved intestinal segments can be resected. Colonoscopy can be employed to snare polyps within reach.
Prognosis
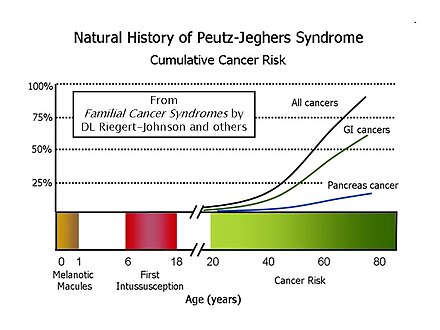
Most patients with PJS will develop flat, brownish spots (melanotic macules) on the skin, especially on the lips and oral mucosa, during the first year of life. The first bowel obstruction due to intussusception usually occurs between the ages of six and 18. The cumulative lifetime cancer risk increases in middle age, with risks by age 70 for all cancers, gastrointestinal cancers, and pancreatic cancer being 85%, 57%, and 11%, respectively.
A Dutch study followed 133 patients for 14 years, finding a cumulative cancer risk of 40% at age 40 and 76% at age 70. Mortality was higher compared to the general population, with cancer being the leading cause of death at a median age of 45.
Monitoring

Suggestions for cancer surveillance include small bowel radiography every two years, esophagogastroduodenoscopy and colonoscopy every two years, yearly CT scan or MRI of the pancreas, yearly ultrasound of the pelvis and testes, annual mammography starting at age 25, and annual Papanicolaou smear (Pap smear) beginning at age 18-20. Follow-up care should be supervised by a physician familiar with PJS, and genetic consultation along with urological and gynaecological consultations is often necessary.
Eponym
Peutz–Jeghers syndrome was first described in a case report in 1921 by Dutch Internist Jan Peutz. It was later formalised into the syndrome by American physicians Harold Joseph Jeghers, Kermit Harry Katz, and Victor Almon McKusick in 1949 and published in the New England Journal of Medicine.
Self-assessment MCQs (single best answer)
Peutz–Jeghers syndrome (PJS) is primarily characterised by which of the following?
What is the estimated incidence of Peutz–Jeghers syndrome?
Which gene is associated with Peutz–Jeghers syndrome?
What is the pattern of inheritance for Peutz–Jeghers syndrome?
What is the lifetime risk of colorectal cancer in patients with Peutz–Jeghers syndrome?
Which of the following is NOT a common site for hyperpigmented macules in Peutz–Jeghers syndrome?
Patients with Peutz–Jeghers syndrome are recommended to undergo small bowel radiography at what frequency?
Which type of tumour is notably associated with an increased risk in females with Peutz–Jeghers syndrome?
At what age does the first bowel obstruction due to intussusception typically occur in Peutz–Jeghers syndrome?
What is a key component of the clinical diagnosis of Peutz–Jeghers syndrome?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


