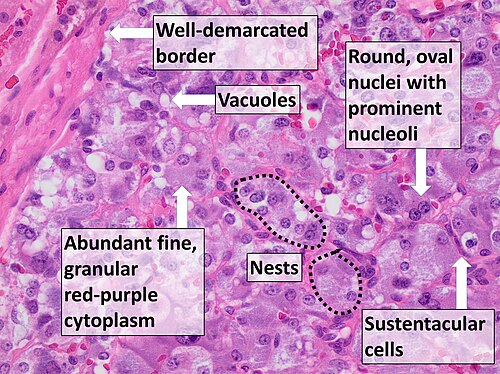
Pheochromocytoma
Pheochromocytoma is a rare neuroendocrine tumour of the adrenal medulla, composed of chromaffin cells. It belongs to the paraganglioma (PGL) family of tumours and can be either intra-adrenal or extra-adrenal. These tumours often secrete catecholamines, leading to a range of symptoms and complications.

Signs and Symptoms
The symptoms of pheochromocytoma are primarily due to the excessive secretion of catecholamines, manifesting as:
- Hypertension (high blood pressure)
- Tachycardia (fast heart rate)
- Diaphoresis (excessive sweating)
- Headaches
Other symptoms include pallor, heat intolerance, weight loss, chest/abdominal discomfort, palpitations, nausea, vomiting, constipation, orthostatic hypotension, and psychiatric symptoms like anxiety and panic attacks.

Complications can be severe, including hypertensive crises, myocardial infarctions, toxic myocarditis, cardiomyopathy, arrhythmias, strokes, acute renal failure, and multiple organ dysfunction syndrome (MODS).
Diagnosis
Biochemical Evaluation
Elevated plasma free metanephrines are the gold standard for diagnosing pheochromocytoma. Additional tests include urinary metanephrines, plasma catecholamines, and Chromogranin A levels. Conditions for accurate testing involve patient rest, medication adjustments, and dietary restrictions.
Imaging
Anatomic imaging with computed tomography (CT) or magnetic resonance imaging (MRI) is used to locate the tumour. Functional imaging techniques, such as 18F-FDG PET, 123I-MIBG, 18F-FDOPA, and 68Ga-DOTA, help characterise the tumour and detect metastases.

Treatment
Surgery
Surgical resection is the only curative option. The preferred method for adrenal tumours is laparoscopic adrenalectomy unless the tumour is invasive or larger than 6 cm. Pre-operative management involves alpha-adrenoceptor blockade to prevent catecholamine crises during surgery. Selective alpha-1 adrenoceptor antagonists (e.g., doxazosin) or non-selective agents (phenoxybenzamine) are used based on the patient's blood pressure. Beta-blockers are added for tachycardia.
Post-operative Management
Post-surgical complications include hypertension, hypotension, hyperglycaemia, hypoglycaemia, and adrenal insufficiency. Ensuring adequate fluid intake and monitoring blood glucose levels are very important.
Metastatic Disease
Metastatic pheochromocytoma often involves the lymph nodes, lungs, liver, and bones. Treatment options include surgery, radiation therapy, chemotherapy, and radionuclide therapy. Surgery aims to debulk the tumour, while radiation therapy is used for pain control and local disease management. Chemotherapy regimens like CVD (cyclophosphamide, vincristine, and dacarbazine) and temozolomide (TMZ) are employed. Radionuclide therapies, including iodine-131 meta-iodobenzylguanadine (MIBG) and peptide receptor radionuclide therapy (PRRT), are also effective.

Genetics
Approximately 40% of pheochromocytomas are related to inherited germline mutations. Genetic counselling and testing are recommended for all patients. Common hereditary syndromes include MEN2, VHL, and NF1, each with distinct clinical characteristics and associated tumour risks.
Hereditary Syndromes
MEN2 (RET): Associated with medullary thyroid carcinoma, hyperparathyroidism, and pheochromocytoma.
VHL (VHL): Linked to renal cell carcinoma, pancreatic NET, and retinal/CNS hemangioblastoma.
NF1 (NF1): Characterised by neurofibromas, cafe-au-lait macules, and pheochromocytoma.
Self-assessment MCQs (single best answer)
What is the primary cause of symptoms in pheochromocytoma?
Which imaging technique is considered the gold standard for locating a pheochromocytoma?
Which of the following is NOT a common symptom of pheochromocytoma?
What is the preferred surgical method for adrenal tumours in pheochromocytoma?
Which genetic syndrome is associated with medullary thyroid carcinoma, hyperparathyroidism, and pheochromocytoma?
What is the primary biochemical test for diagnosing pheochromocytoma?
Which radionuclide therapy is used specifically for treating metastatic pheochromocytoma?
Which of the following is a potential post-operative complication after resecting a pheochromocytoma?
What is the most common site for metastatic spread of pheochromocytoma?
Which of the following symptoms is associated with orthostatic hypotension in pheochromocytoma?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


