Rectal Prolapse
Introduction
Rectal prolapse is a medical condition where the walls of the rectum protrude through the anus, becoming visible externally.
This condition can manifest in various forms and severities, affecting both sexes, although it is more prevalent in elderly women. Rectal prolapse can range from being asymptomatic to causing significant discomfort and impairment.
Classification
Rectal prolapse can be classified based on several factors:
- Full thickness (complete) vs. Mucosal (partial): Full thickness involves all rectal wall layers, whereas mucosal involves only the mucosal layer.
- External vs. Internal: External prolapse is visible from the anus, while internal prolapse does not protrude externally.
- Circumferential vs. Segmental: Circumferential involves the whole rectal circumference, and segmental involves parts.
- Present at rest vs. During straining: The prolapse may present without any activity or only during straining.
Signs and Symptoms
Symptoms of rectal prolapse include:
- Protruding mass from the anus.
- Faecal incontinence, often presenting as mucous discharge.
- Constipation or tenesmus.
- Sensation of rectal fullness or bearing down.
- Rectal bleeding and erratic bowel habits.

Diagnosis
History and Physical Examination
A thorough history and physical examination are very important. Rectal prolapse can be confused with prolapsing haemorrhoids. Full thickness rectal prolapse is identified by circumferential folds, while mucosal prolapse has radial folds. The anus may appear patulous and have reduced resting and squeeze pressures.
Proctoscopy/Sigmoidoscopy/Colonoscopy
These procedures can reveal mucosal congestion, oedema, or a solitary rectal ulcer. They help in ruling out colorectal cancer, which is more prevalent in the elderly.
Videodefecography
This imaging technique is used to diagnose internal intussusception or confirm external prolapse not evident during a physical exam.
Colonic Transit Studies and Anorectal Manometry
These studies assess colonic inertia and sphincter functionality, respectively, which can influence treatment decisions.

Treatment
Conservative Management
For patients unfit for surgery or with minimal symptoms, conservative measures such as dietary adjustments to increase fibre intake and stool softeners can be beneficial to reduce straining during defecation.
Surgical Management
Surgery is often required to prevent further damage and alleviate symptoms. The approach can be either abdominal or perineal.
Abdominal Procedures
Abdominal operations, including laparoscopic techniques, are associated with lower recurrence rates. They involve rectopexy and/or resection of the rectum. Laparoscopic procedures are preferred due to their shorter recovery times and less postoperative pain.
Perineal Procedures
Perineal approaches like perineal rectosigmoidectomy (Altemeier procedure) and the Delorme procedure are less invasive and preferred for elderly or high-risk patients. The Thiersch procedure is used for severely impaired patients, involving the placement of a subcutaneous suture around the anus to prevent prolapse.
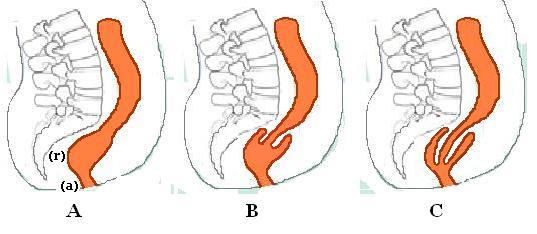
Internal Rectal Intussusception
Internal rectal intussusception involves the infolding of the rectal wall and can cause symptoms like faecal leakage, obstructed defecation, and pelvic pain. Diagnosis is often made using defecography or dynamic MRI defecography. Treatment options include conservative measures such as pelvic floor retraining and biofeedback or surgical interventions like laparoscopic ventral (mesh) rectopexy and stapled trans-anal rectal resection (STARR).
Mucosal Prolapse
Mucosal prolapse refers to the descent of the rectal mucosa through the anus. It can cause symptoms like faecal leakage, rectal bleeding, mucous discharge, and pain. Treatment involves examination under anaesthesia and banding of the mucosa.
Solitary Rectal Ulcer Syndrome (SRUS)
SRUS is caused by straining and increased pressure during defecation, leading to rectal ulceration. Symptoms include straining, mucous discharge, rectal bleeding, and a sensation of incomplete evacuation. Treatment focuses on reducing straining and may include biofeedback and surgery if conservative measures fail.
Conclusion
Rectal prolapse encompasses a range of conditions with varying severity and treatment options. Proper diagnosis and individualised treatment plans are essential for effective management.
Self-assessment MCQs (single best answer)
What is rectal prolapse?
Which of the following is more common in elderly women?
What distinguishes full thickness rectal prolapse from mucosal prolapse?
Which imaging technique is used to diagnose internal intussusception?
What symptoms might indicate rectal prolapse?
Which surgical procedure is preferred for elderly or high-risk patients with rectal prolapse?
What symptom is commonly associated with internal rectal intussusception?
Which of the following is a conservative treatment for rectal prolapse?
What is the main goal of treatment for Solitary Rectal Ulcer Syndrome (SRUS)?
Which of the following procedures involves placing a subcutaneous suture around the anus to prevent prolapse?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


