Rubinstein–Taybi Syndrome (RTS)
Rubinstein–Taybi Syndrome (RTS), also known as Broad thumb-hallux syndrome or Rubinstein syndrome, is a rare genetic condition characterised by short stature, moderate to severe learning difficulties, distinctive facial features, and broad thumbs and first toes.
The condition is primarily caused by a mutation or deletion in the CREBBP gene on chromosome 16, and/or the EP300 gene on chromosome 22. These genetic anomalies lead to a range of physical and cognitive symptoms, varying among affected individuals.
Presentation

RTS manifests from birth and is usually marked by delayed physical and cognitive growth. Typical features of the disorder include broad thumbs, broad first toes, and clinodactyly of the fifth finger. Patients often have a small stature, low bone growth, and a small head. Male patients may exhibit cryptorchidism. Unusual facial characteristics involving the eyes, nose, and palate are common.

Anaesthesia may pose risks for these patients due to potential complications such as respiratory distress and cardiac arrhythmias. Children with RTS are more likely to be overweight and may exhibit a short attention span, motor stereotypies, and poor coordination, possibly due to the impaired motor skills learning associated with the CREBBP gene. Evidence also suggests a link with long-term memory deficits.
Genetics
RTS is often a microdeletion syndrome involving the chromosomal segment 16p13.3, characterised by mutations in the CREBBP gene. The CREBBP gene produces a protein that helps control the activity of many other genes, playing a essential role in regulating cell growth and division, and is essential for normal foetal development.
Mutations in the EP300 gene on chromosome 22q13.2 are responsible for a smaller percentage of RTS cases. These mutations result in the loss of one copy of the gene in each cell, reducing the amount of p300 protein by half, leading to disrupted normal development.
In about one-third of the cases exhibiting RTS symptoms, neither the CREBBP nor the EP300 genes appear to be responsible for the disease. A mouse model displaying the same clinical RTS symptoms seen in humans has been identified for research purposes.
Diagnosis
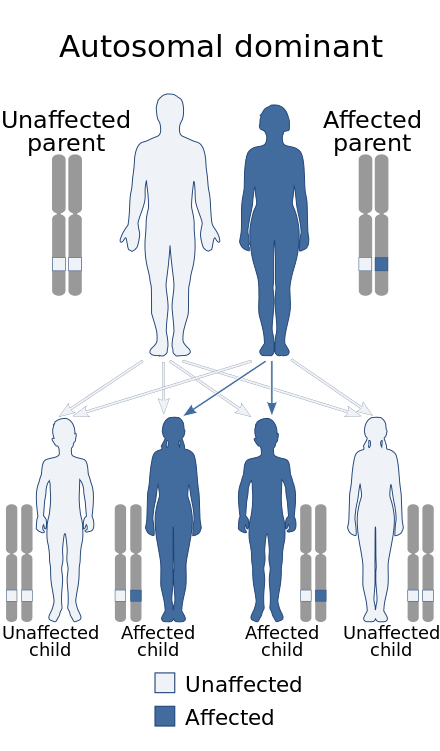
RTS is diagnosed when a heterozygous pathogenic variant of the CREBBP gene is identified in an individual, exhibiting an autosomal dominant inheritance pattern. Some cases show heterozygous individuals exhibiting germline mosaicism. The condition affects men and women equally and is often misdiagnosed with other diseases or disabilities causing delayed mental development.
Treatment
There is no treatment to reverse or cure RTS. Management focuses on reducing symptoms specific to each patient, who may suffer from a diverse range of symptoms. Patients are referred to specialists for their specific symptoms, such as orthopaedic surgeons and physical therapy for skeletal and growth abnormalities, cardiologists for heart abnormalities, and dentists for dental abnormalities.
Cognitive developments are typically addressed through special education programmes and speech therapy. Regular check-ups and monitoring are necessary for cardiac, dental, auditory, and renal abnormalities. Genetic counselling is recommended for affected individuals and their families.
History
Rubinstein–Taybi syndrome was first unofficially mentioned in 1957 by Greek physicians in a French orthopaedic medical journal. The syndrome was later formally documented in 1963 by Dr. Jack Herbert Rubinstein and Dr. Hooshang Taybi, who recognised the characteristic features of broad thumbs and toes, unusual facial features, and intellectual disabilities in affected children.
The first genetic abnormalities associated with RTS were identified in 1992, affecting either chromosome 16 or chromosome 22, leading to the classification of RTS into types based on the specific chromosomal mutation.
Self-assessment MCQs (single best answer)
What gene is primarily associated with causing Rubinstein–Taybi Syndrome?
Which chromosome is the CREBBP gene located on?
Which of the following is NOT a common feature of Rubinstein–Taybi Syndrome?
What inheritance pattern does Rubinstein–Taybi Syndrome follow?
Which gene mutation is responsible for a smaller percentage of Rubinstein–Taybi Syndrome cases?
Which physical characteristic is commonly observed in individuals with Rubinstein–Taybi Syndrome?
What is a significant risk when administering anaesthesia to patients with Rubinstein–Taybi Syndrome?
What type of genetic testing confirms a diagnosis of Rubinstein–Taybi Syndrome?
What type of specialist is NOT typically involved in the management of Rubinstein–Taybi Syndrome?
In what year was Rubinstein–Taybi Syndrome formally documented by Dr. Jack Herbert Rubinstein and Dr. Hooshang Taybi?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


