Sarcopenia
Sarcopenia is a medical condition characterised by the degenerative loss of skeletal muscle mass, quality, and strength due to ageing or immobility. It is distinct from cachexia, where muscle degradation occurs through cytokine-mediated pathways, although they may co-exist. Sarcopenia is a significant component of frailty syndrome and can lead to reduced quality of life, falls, fractures, and disability.
Causes
The causes of sarcopenia are multifactorial and include hormonal changes, immobility, age-related muscle changes, nutrition, and neurodegenerative factors. Immobility significantly accelerates muscle loss, even in younger individuals. Other contributing factors include decreased nutrient intake, low physical activity, and chronic diseases. Early environmental influences, such as low birth weight, are also associated with reduced muscle mass and strength in adulthood.
Pathophysiology
Several mechanisms are proposed to explain sarcopenia, including changes in myosatellite cell recruitment, anabolic signalling, protein oxidation, inflammation, and developmental factors. Sarcopenic muscle shows a reduction in muscle tissue quality, increased fibrosis, changes in muscle metabolism, oxidative stress, and degeneration of the neuromuscular junction. Ageing muscles also exhibit an accumulation of mitochondrial DNA mutations and a shift in the types of muscle fibres, with a decrease in type II (fast-twitch) fibres.
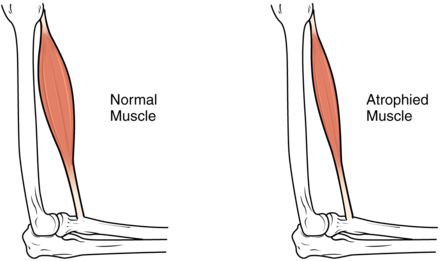
Signs and Symptoms
The hallmark sign of sarcopenia is muscle atrophy or loss of lean muscle mass. This change can be difficult to detect due to obesity, changes in fat mass, or oedema. Weight, limb, or waist circumference are unreliable indicators. Other symptoms include reduced strength, functional decline, and an increased risk of falling. In its early stages, sarcopenia may have no symptoms and is often unrecognised.
Diagnosis
Diagnosis is challenging due to the lack of a universally accepted definition. Sarcopenia can be diagnosed when muscle mass is at least two standard deviations below the population mean, coupled with a slow walking speed. The European Working Group on Sarcopenia in Older People (EWGSOP) suggests the presence of low muscle mass and either low muscular strength or low physical performance as diagnostic criteria. Hand grip strength is often used as a clinical marker due to its simplicity and cost-effectiveness.
Biomarkers
Certain biomarkers are associated with sarcopenia, including increased inflammatory markers (CRP, TNF, interleukins), and reduced sex hormones (testosterone, DHEA sulphate), growth hormone, and IGF-1. Circulating C-terminal agrin fragments (CAF) and lower plasma levels of essential amino acids are also indicative. Low circulating alanine aminotransferase (ALT) is another marker.
Management
Exercise
Exercise is the primary intervention for sarcopenia. Resistance training can improve physical performance, strength, and muscle mass. It increases mitochondrial numbers, capillary density, and connective tissue strength. However, translating research into clinical practice remains challenging due to variability in exercise protocols.
Medication
There are currently no approved medications for sarcopenia. Testosterone and anabolic steroids have shown some efficacy but come with significant side effects. Growth hormone and DHEA have limited effectiveness. Other potential treatments under investigation include ghrelin, vitamin D, ACE inhibitors, and eicosapentaenoic acid.
Nutrition
Adequate calorie and protein intake are very important for muscle protein synthesis. Older adults may require higher protein intake (1.0–1.2 g/kg body weight per day) to prevent muscle atrophy. Ensuring proper nutrition is a low-cost, side-effect-free approach to managing sarcopenia.
Supplements
Amino acid supplementation, particularly leucine, can counteract muscle loss. β-hydroxy β-methylbutyrate (HMB), a leucine metabolite, stimulates protein synthesis and has shown promise in clinical trials for preserving lean body mass in older adults.
Epidemiology
The prevalence of sarcopenia varies but is estimated to affect 5-13% of people aged 60-70 and 11-50% of those over 80. This condition affects over 50 million people and is projected to impact over 200 million in the next 40 years due to the ageing population.
Public Health Impact
Sarcopenia is a growing public health concern due to its association with increased disability, falls, mortality, and healthcare costs. It significantly impacts quality of life and represents a substantial burden on healthcare systems.
Research Directions
Future research should focus on the molecular mechanisms of sarcopenia, refining diagnostic criteria, and developing effective therapeutic interventions. There is an unmet need for anabolic drugs with minimal side effects, as current treatments have not shown sufficient efficacy in improving physical function despite increasing lean mass.
Self-assessment MCQs (single best answer)
What is the ICD-10 code for Sarcopenia?
Which of the following is NOT a proposed mechanism for sarcopenia?
What is the hallmark sign of sarcopenia?
Which organisation suggests using low muscle mass and either low muscular strength or low physical performance for diagnosing sarcopenia?
What is a common clinical marker used in the diagnosis of sarcopenia due to its simplicity and cost-effectiveness?
Which of the following is NOT currently an approved medication for sarcopenia?
What is the recommended daily protein intake for older adults to prevent muscle atrophy?
Which metabolite of leucine has shown promise in clinical trials for preserving lean body mass in older adults?
According to the text, what percentage of people aged 60-70 are estimated to be affected by sarcopenia?
Which of the following is NOT a focus for future research on sarcopenia?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


