Thrombotic Thrombocytopenic Purpura
Thrombotic thrombocytopenic purpura (TTP), also known as Moschcowitz syndrome or idiopathic thrombotic thrombocytopenic purpura, is a blood disorder characterised by the formation of blood clots in small blood vessels throughout the body.
This condition leads to a low platelet count, hemolytic anaemia due to red blood cell breakdown, and potential dysfunction of the kidneys, heart, and brain. The disorder predominantly affects adults, with women being more commonly impacted than men.

Signs and Symptoms
The early signs and symptoms of TTP can be subtle and nonspecific, often resembling an influenza-like illness or a diarrheal episode. Common neurological symptoms include fatigue, confusion, and headaches, with more severe manifestations such as seizures and stroke-like symptoms. Other symptoms involve jaundice, paleness of the skin, a fast heart rate, shortness of breath, and the presence of petechiae (small red or purple spots on the skin). High blood pressure is also commonly observed. As TTP progresses, blood clots in small vessels lead to the consumption of platelets, resulting in bruising and occasionally bleeding, with larger bruises (ecchymoses) forming less frequently.
The classic presentation of TTP, though rare (less than 10% of cases), includes five key medical signs:
- Fever
- Changes in mental status
- Thrombocytopenia
- Reduced kidney function
- Hemolytic anaemia
Causes
TTP is primarily caused by the spontaneous aggregation of platelets and the activation of coagulation in small blood vessels. The two main types of TTP are autoimmune (acquired TTP) and congenital (Upshaw–Schulman syndrome).
Autoimmune
In many cases, TTP is caused by autoantibodies that inhibit the enzyme ADAMTS13, responsible for breaking down von Willebrand factor (vWF). Without proper cleavage by ADAMTS13, large multimers of vWF lead to increased coagulation, particularly in the microvasculature. Two independent research groups identified this relationship in 1998.
Genetic
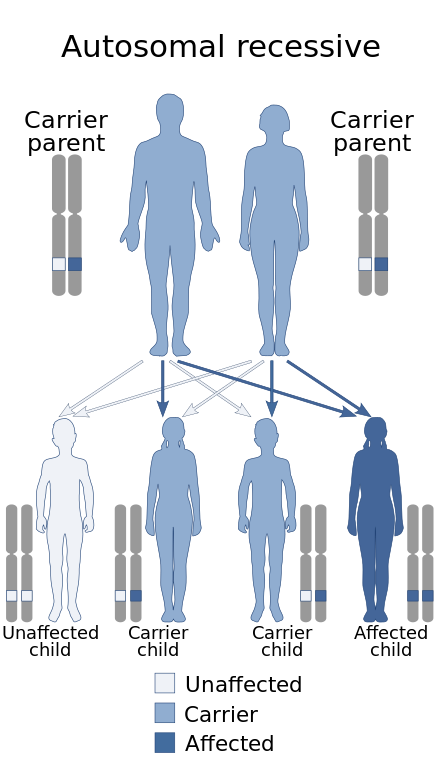
Congenital TTP, known as Upshaw–Schulman syndrome, is caused by mutations in the ADAMTS13 gene, leading to a deficiency from birth. Individuals with this syndrome often have mild symptoms but may develop TTP during infections or other stressors.
Secondary
Secondary TTP is associated with various conditions such as cancer, bone marrow transplantation, pregnancy, and the use of certain medications. The exact mechanism of secondary TTP is not well understood, though endothelial damage and vessel occlusion may play roles.
Diagnosis
Diagnosing TTP involves recognising the characteristic symptoms and conducting blood tests. A key diagnostic marker is the ADAMTS13 activity level, with ≤5% of normal activity indicating TTP. Differential diagnosis includes differentiating TTP from other thrombotic microangiopathies (TMAs) like hemolytic-uraemic syndrome (HUS) and atypical hemolytic uraemic syndrome (aHUS).
Treatment
Due to the high mortality rate of untreated TTP, immediate treatment is very important. Plasma exchange (plasmapheresis) is the treatment of choice, involving daily removal of the patient’s plasma and replacement with donor plasma. Corticosteroids and rituximab may also be used to reduce antibody production. Caplacizumab has been shown to induce faster disease resolution but may increase bleeding tendencies.
In cases of refractory or relapsing TTP, additional immunosuppressive therapies or splenectomy may be required. For congenital cases, prophylactic plasma infusions are administered regularly.
Prognosis
The mortality rate for untreated TTP is around 95%, but with early diagnosis and treatment, the survival rate improves significantly to 80-90%. Depression is common among recovered patients, with many screening positive within 11 years post-recovery.
Epidemiology
TTP affects approximately 1 in 100,000 people annually, with a higher incidence in women and individuals of African descent. It is also notably associated with pregnancy, affecting about one in 25,000 pregnancies.
History
TTP was first described by Eli Moschcowitz in 1924. Initial treatments were limited, but the introduction of plasma exchange in the early 1990s significantly improved survival rates. The identification of ADAMTS13 as a key factor in the disease mechanism was made in the late 1990s.
Self-assessment MCQs (single best answer)
Which of the following is NOT a common symptom of TTP?
What enzyme is inhibited by autoantibodies in autoimmune TTP?
TTP is most commonly found in which demographic group?
Which of the following is the primary treatment for TTP?
In the context of TTP, what does the presence of petechiae indicate?
Which of the following conditions is NOT typically associated with secondary TTP?
How is congenital TTP (Upshaw–Schulman syndrome) inherited?
What key diagnostic marker is used to indicate TTP?
Who first described TTP in 1924?
What is the survival rate for TTP with early diagnosis and treatment?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


