Thymoma
A thymoma is a rare malignancy that originates from the epithelial cells of the thymus. It is often associated with neuromuscular disorders such as myasthenia gravis (MG), with 20% of MG patients having a thymoma. Thymomas primarily affect adults and are treated through surgical removal. Chemotherapy is reserved for malignant cases.
Signs and Symptoms
Approximately one-third of patients with thymoma exhibit symptoms caused by the compression of surrounding organs by the tumour mass. These symptoms can include superior vena cava syndrome, dysphagia (difficulty swallowing), cough, or chest pain. Another third of patients discover their tumour due to associated autoimmune disorders, the most common being myasthenia gravis.
Other autoimmune conditions linked with thymoma include pure red cell aplasia, Good syndrome, and thymoma-associated multiorgan autoimmunity.
Additional associations include acute pericarditis, agranulocytosis, alopecia areata, ulcerative colitis, Cushing's disease, hemolytic anaemia, limbic encephalopathy, myocarditis, nephrotic syndrome, panhypopituitarism, pernicious anaemia, polymyositis, rheumatoid arthritis, sarcoidosis, scleroderma, stiff person syndrome, systemic lupus erythematosus, and thyroiditis.
A significant proportion of patients (one-third to one-half) are asymptomatic, and the tumour is discovered incidentally through imaging performed for other reasons.
Pathology
Thymomas originate from thymic epithelial cells. They are classified into three principal histological types based on microscopic appearance:
- Type A: Epithelial cells have an oval or fusiform shape with fewer lymphocytes.
- Type B: Epithelial cells have an epithelioid shape and are subdivided into:
- B1: Lymphocyte-rich
- B2: Cortical
- B3: Epithelial
- Type AB: Contains a combination of both cell types.
Thymomas are further characterised by the features of thymic cortical or medullary epithelial cells, influencing their benign or malignant nature.
Diagnosis


When thymoma is suspected, a CT/CAT scan is performed to determine the size and extent of the tumour. A CT-guided needle biopsy is typically used for sampling. Increased vascular enhancement and pleural deposits on CT scans can indicate malignancy. The diagnosis is confirmed through histologic examination by a pathologist using a tissue sample. The Masaoka Staging System is used to classify the tumour based on the extent of disease at the time of surgery:
- I: Completely encapsulated
- IIA: Microscopic invasion through the capsule into surrounding fatty tissue
- IIB: Macroscopic invasion into the capsule
- III: Macroscopic invasion into adjacent organs
- IVA: Pleural or pericardial implants
- IVB: Lymphogenous or hematogenous metastasis to distant sites
Treatment
Surgical removal is the primary treatment for thymoma. In cases of invasive and large tumours, neoadjuvant chemotherapy and/or radiotherapy may be employed to reduce tumour size before surgery. For early-stage tumours (Masaoka I through IIB), no additional therapy is required. Invasive thymomas may necessitate further treatment with radiotherapy and chemotherapy. Recurrences can occur in 10-30% of cases, and pleural recurrences may be surgically removed followed by hyperthermic intrathoracic perfusion chemotherapy.
Prognosis
Prognosis varies significantly with the stage of the tumour. Stage III or IV thymomas have a much worse prognosis compared to stage I and II tumours. Thymomas rarely metastasize, but when they do, common sites include the pleura, bones, liver, and brain. Approximately 40% of patients with stage III and IV thymomas survive for at least 10 years after diagnosis, with a median diagnosis age of 57 years.
Epidemiology
Thymomas have an incidence of about 0.13-0.26 per 100,000 people per year, with a slightly higher prevalence in females. The typical age at diagnosis ranges from the 40s to 50s, although cases have been reported from six to 83 years.
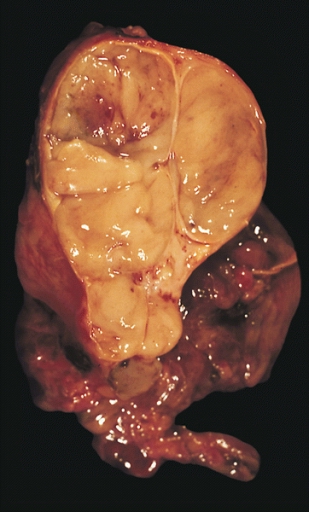
Gallery






Self-assessment MCQs (single best answer)
What is the primary treatment for thymoma?
Which autoimmune disorder is most commonly associated with thymoma?
What is the typical age range for thymoma diagnosis?
Which histological type of thymoma is characterised by oval or fusiform epithelial cells with fewer lymphocytes?
In the Masaoka Staging System, what stage is characterised by microscopic invasion through the capsule into surrounding fatty tissue?
What imaging modality is primarily used to determine the size and extent of a suspected thymoma?
Which of the following symptoms is NOT typically caused by the compression of surrounding organs by a thymoma?
What percentage of myasthenia gravis patients have a thymoma?
Which of the following is NOT a histological subtype of Type B thymoma?
What is the incidence of thymomas per 100,000 people per year?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!


